Announcement
Vascular Cell encourages submission of manuscripts evaluating the link between Covid-19 and cardiovascular system.The articles will be evaluated within 48 h and if accepted, after the review process, they will be published free of charge.
Please read further instructions regarding the style and formatting of the manuscript in the Information for Readers section.
Aims and scope
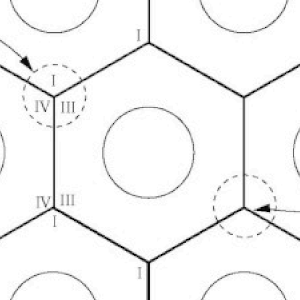
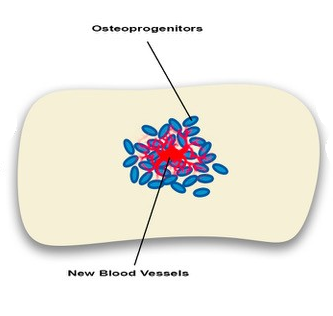
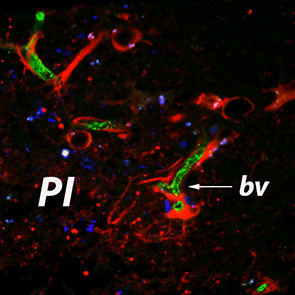
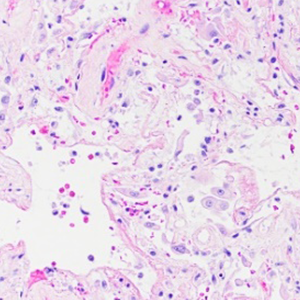
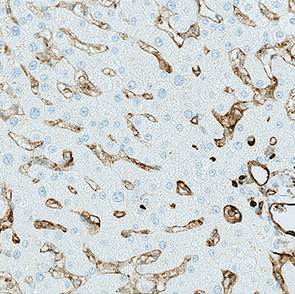
Vascular Cell represents an open access medical journal which concentrates on publication of a wide range of topics related to the vascular system including neo-vascularization and angiogenesis. Since vascular endothelial cells represent a crucial factor in numerous pathological conditions such as: cancer, stroke, myocardial infarction or atherosclerosis their behavior is of paramount importance for the clinical outcomes of a wide range of patients.
VascularCell indexing
We are in the process of reindexing VascularCell with PubMed. Currently PubMed holds the archive of Vascular Cell articles published between 2009-2017
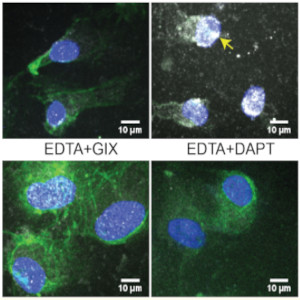
Latest Articles
VascularCell articles from Volume 14 (issue 1), published in 2023.